Pain control is just one of those skills that specifies the high quality of frontline care. When a patient is squirming on the flooring of a manufacturing facility, or a kid is worried after a compound fracture at a weekend break game, you do not have lengthy to make sound choices. PUAEME008, Give Discomfort Management, codifies what skilled -responders must do to assess discomfort, pick and supply secure analgesia, display outcomes, and turn over treatment. It is more than a system of expertise. It is a small between a medical professional and a client in distress.
I have actually supplied and assessed this unit for combined teams, from remote mine medics to metropolitan occasion paramedics, and the exact same styles come up every program: recognize your pharmacology and contraindications, regard consent and law, always remember non‑pharmacological care, and file as if another person will need to run with the baton ten mins later. This write-up unboxes PUAEME008 in practical terms and offers a functioning picture of what skilled efficiency resembles in genuine environments.
Where PUAEME008 Sits in Practice
PUAEME008 beings in the Public Safety And Security Training Bundle and is generally packaged right into discomfort administration programs run by signed up training organisations for emergency -responders and allied health professionals working in ascetic or prehospital contexts. Learners are generally already trained in primary survey, respiratory tract management, basic life assistance, and scene safety and security. The give pain management program builds on that structure to attend to risk-free, reliable analgesia across a range of patients and environments.
Providers vary throughout Australia. Some supply the device as a standalone pain administration certificate program, others fold it into wider programs like remote area initial responder training. For nurses and physio therapists who work in occasion medication, occupational health, or remote outreach, it can enhance professional registration by formalising prehospital analgesia skills. It is not a substitute for a tertiary pain fellowship. Instead, it is a concentrated emergency situation pain management module that asks an essential concern: can you eliminate pain swiftly and securely while preparing for deterioration?
The Proficiency at a Glance
PUAEME008 assessors search for clear, observable efficiency. The phrasing varies somewhat across variations, but the core needs stay steady:
- Recognise and assess acute pain utilizing structured devices fit to the client and situation. Select ideal analgesic methods, consisting of non‑pharmacological techniques, according to procedures, range of technique, and offered resources. Administer analgesia safely using approved routes, dosages, and devices while preserving infection control. Monitor response, adverse effects, and essential indicators, after that titrate or discontinue treatment accordingly. Communicate plainly, gain consent, file, and turn over to a greater level of care.
These components sound tidy theoretically. Actual scenes are not. You will evaluate a patient with disruptive injuries and a windstorm blowing sand right into your eyes. You will look for a radial pulse while a group movies on their phones. Competence receives exactly how you build a quick yet reliable photo, keep the client involved and tranquility, and use a procedure without passage vision.
Assessment and Triage: Reading Pain, Not Thinking It
Pain is subjective and greatly coloured by worry, society, and context. A jackaroo with a dislocated shoulder could rate his pain at 6 yet look pale and clammy with a heart rate of 130. A kid might reject to talk yet wince with a light touch. PUAEME008 anticipates responders to make use of discomfort scales that fit the patient. The numerical rating range from 0 to 10 suits verbalize adults. The Wong‑Baker deals with scale assists in interaction with youngsters or patients that prefer visual hints. For non‑verbal individuals, behavioural tools such as the FLACC range help, though they require method to avoid overcalling distress as pain.
Acute discomfort assessment in the field must not drift into a lengthy interview. Anchor it within the key and additional surveys. Begin with life risks, then a focused discomfort history: location, start, personality, radiation, severity, time training course, exacerbating or easing variables, and previous anesthetics. Pulse oximetry, heart price, respiratory system rate, high blood pressure, and skin indicators supply context. Keep in mind warnings that alter the plan: altered psychological state, suspected major hemorrhage, chest discomfort with hemodynamic instability, severe head injury, or indications of blood poisoning. PUAEME008 desires -responders to identify when analgesia is necessary and when support of air passage, breathing, and circulation has to precede it by mins that feel much longer.
Anecdotally, one of the most common analysis error from brand-new learners is stopping working to reassess. They capture a baseline pain score, deliver an opioid, then carry on with other tasks. 10 minutes later the discomfort has actually held one's ground, yet since no organized reassessment happened, the possibility to titrate is lost. Excellent technique is basic. Tape a pain rating prior to treatment, however every 5 to 10 mins or after each dose. Pair it with vitals and an observation of sedation degree, so you can detect respiratory system clinical depression early.

Pharmacological Choices: What remains in the Set and When to Use It
The provide pain administration program teaches pharmacological options aligned to organisational methods. Accessibility differs. Remote clinics might stock methoxyflurane, intranasal fentanyl, paracetamol, and advil. Event medics may operate under standing orders for oral anesthetics only. Paramedic services include IV morphine, ketamine, and occasionally nitrous oxide.
Paracetamol continues to be the quiet workhorse. At restorative dosages it decreases discomfort in musculoskeletal injuries and soft cells injury. It likewise pairs well with NSAIDs for a synergistic result. Look for current intake to avoid advancing toxicity, especially in smaller sized grownups or those with liver disease. Ibuprofen and other NSAIDs bring anti‑inflammatory advantages however lug bleeding and renal risks. Post‑operative clients, the elderly with poor kidney book, and people on anticoagulants could be better offered by different strategies.
Methoxyflurane, delivered using a portable inhaler, has a devoted complying with in the field. Its fast beginning and patient‑controlled nature fit short, painful procedures like lowering a disjointed shoulder or splinting a crack. Expect sedation, hypotension, and the advancing dose restriction. Several methods cap it at two 3 millilitre vials in 24 hr. I have had clients who barely touched the inhaler after the first minute due to the fact that focused coaching and splinting alleviated. Others needed the complete allocation to assist in extrication. It is tempting to get along with strategies while the patient is patient, however if their vitals trend inadequately, stop and reassess before continuing.
Intranasal fentanyl bridges an essential void when IV access is not possible. Correct dosing based on person weight and shipment through a mucosal atomisation device returns quick analgesia. It is specifically helpful in paediatrics where cannulation hold-ups care. In spite of the comfort, treat it with the respect you would certainly any kind of opioid. Know your contraindications, display respiration, and have naloxone prepared, drawn up, and around. 2 percent of pupils forget to prime the atomiser throughout simulations, which decreases efficacy. Construct a habit of a fast equipment checklist before administration.
IV opioids continue to be staples for many solutions. Titrated increments of morphine or fentanyl permit accurate control. I like little boluses connected to duplicated discomfort scores and sedation analyses as opposed to big front‑loaded dosages, especially for older grownups. Ketamine uses a dissociative path for serious discomfort, specifically in trauma where hypotension looms. Reduced dosage ketamine for analgesia varies from induction doses utilized in step-by-step sedation. Nystagmus and dissociation can agitate the individual and spectators, so comprehensive pre‑briefing aids. I have actually found that tranquil narration throughout administration lowers the opportunity the individual will certainly stress as the medicine takes effect.
Nitrous oxide still shows up at some occasions. It is exceptional for short, sharp treatments, yet logistics and contraindications complicate its use. Expectant patients, those with bowel obstruction, pneumothorax, or caught gas worries should not receive it. Cyndrical tube monitoring at a jampacked site becomes a second threat if not controlled.
Whichever agents you carry, PUAEME008 anchors technique in clear methods and scope. Do not improvisate past training and authorisation, even when stress installs. If your pain administration training program covered intranasal fentanyl and you function under a contract that allows it, you are on solid ground. If ketamine is not in your practice version, the best selection is to rise or seek extra support, not to press boundaries.
Non medicinal Techniques: Often Faster, Always Cheaper
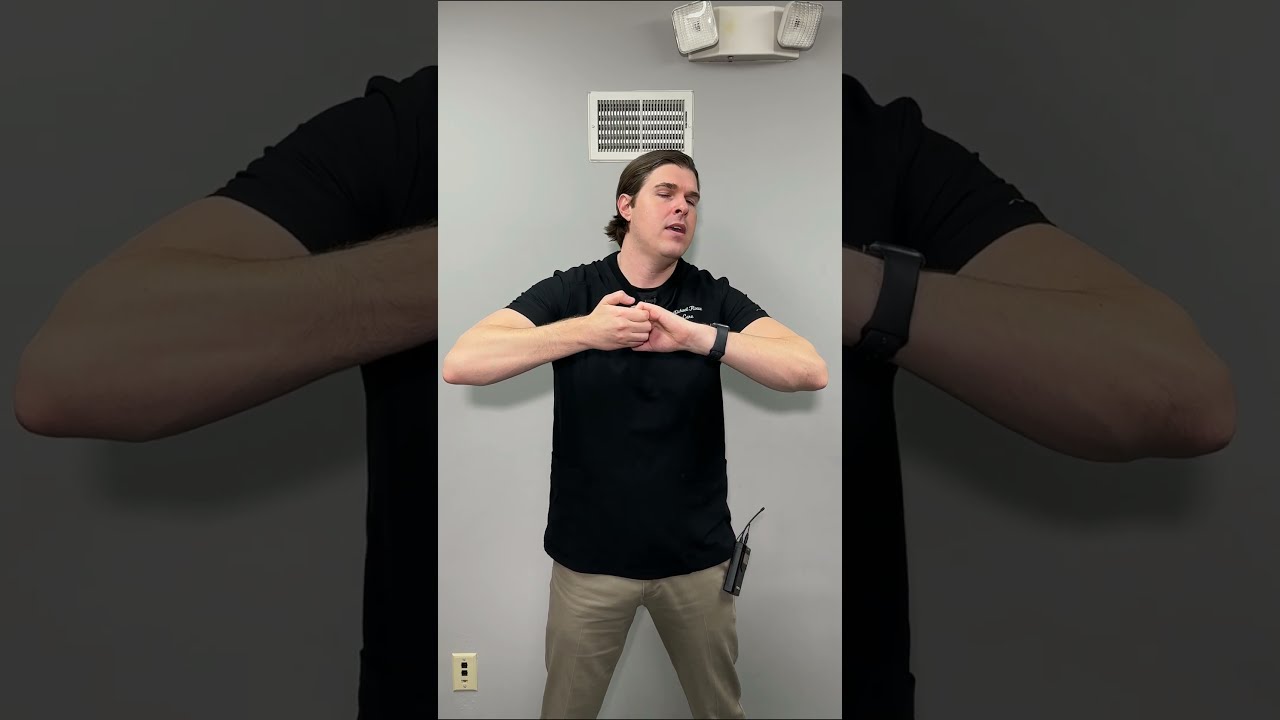
I have watched an anxious individual's pain drop from eight to four within 2 minutes with nothing more than an excellent splint, a warm blanket, and regulated breathing. We talk about drugs due to the fact that they seem like activity, yet fundamental procedures matter.
Immobilisation and splinting continue to be the most powerful non‑drug interventions for trauma discomfort. Effectively cushioned, well positioned splints reduce movement and muscular tissue convulsion. Gentle traction in presumed lengthy bone cracks can relieve the worst of it also before conclusive care. Cold therapy decreases swelling and numbs surface tissues when made use of judiciously. Warm can assist muscular tissue spasm, however avoid it on fresh traumatic injuries.
Positioning slides under the radar. A person with kidney rock discomfort usually discovers alleviation crinkled on one side. Rib cracks really feel much better with the breast a little elevated and supported. Motivate placements that reduce muscle mass pressure, offered back injury is not thought. Basic breathing coaching decreases considerate drive and enhances resistance. I use a 3 matter in, 6 count out rhythm to promote parasympathetic tone, tuned to the client's comfort. Include distraction. Led images seems soft up until you see a youngster with a forearm fracture clear up enough for cannulation because you inquired about their dog and the next football match.
Non pharmacological treatment is where physio therapists and nurses bring huge value. Discomfort administration programs for physio therapists usually stress motion strategies that reduce pain without surging stress and anxiety, and registered nurses bring a second sight for placing and reassurance that pays returns. PUAEME008 anticipates responders to show these steps together with pharmacology, not as an alleviation prize when the medication kit is light.
Consent, Interaction, and Social Safety
Consent can not be a rushed checkbox. Virtually every field mistake I have actually examined after an adverse response entailed inadequate pre‑briefing. Prior to you deliver any kind of analgesia, describe what you plan to do, why, what the individual could really feel, and what side effects to look for, after that ask for consent. Grownups with capacity can refuse discomfort relief even if you think it remains in their passion. File the conversation.
Cultural safety issues. Prevent assumptions about discomfort expression. Some patients will certainly underreport discomfort to meet viewed assumptions. Using neutral, open language assists. Rather than asking "Is it a 10 out of 10?", attempt "Can you show me on this range exactly how solid the discomfort feels right now?" For Initial Nations people, welcome a support person when possible and bear in mind gendered care choices in some areas. Time invested making count on is hardly ever lost and often shortens the overall time to reliable alleviation due to the fact that the client involves with your plan.
Paediatrics and older grownups need unique interest. With children, approval includes moms and dads or guardians, but the kid is worthy of an age‑appropriate explanation and acceptance. Older grownups metabolise medicines in a different way, and polypharmacy rises danger. Halve the preliminary dose, titrate gradually, and keep a hawk's eye on respiration. I have stood in lengthy transportation lines up throughout heatwaves where a little second dose of an opioid tipped a sickly client from comfortable to precariously drowsy. Procedures frequently enable half doses for older grownups. Usage that flexibility.
Monitoring and Handling Negative Effects
Monitoring is the spinal column of secure analgesia. Record standard vitals and repeat at periods suited to the medicine's start and height. Opioids demand respiration price and depth checks, oxygen saturation trends, signs of respiratory tract blockage, and sedation degree. Ketamine calls for high blood pressure, heart price, nystagmus monitoring, emergence reactions, and queasiness. Methoxyflurane calls for focus to level of consciousness and blood pressure. Non‑opioid representatives are not free passes. NSAIDs carry GI bleeding and renal stress danger, though these emerge over longer horizons. Expect allergy with any kind of agent.
Adverse impacts happen, despite having excellent strategy. The metric of capability is not avoiding every event. It is recognition and puaeme008 crucial management. If a person becomes overly sedated after fentanyl, quit dosing, sustain the respiratory tract, use additional oxygen, and ready bag‑valve‑mask support. If air flow is insufficient or oxygen saturation falls despite airway maneuvers, utilize naloxone per procedure. I teach pupils to pre‑calculate the naloxone dosage for their client promptly after administering an opioid, and to verbalise the location of the ampoule. Under tension, this small behavior maintains your action determined as opposed to frantic.
Nausea is common, especially with opioids and methoxyflurane. Have antiemetics easily accessible and place a vomit bag in the person's hands. Lightheadedness and orthostatic drops in stress frequently settle with placing and liquids, if protocols allow. Keep an eye on the clock. Drugs have half lives, and transportation times can be deceptive. If you carry out analgesia right before handover, connect that clearly so the obtaining medical professional comprehends the timing and can prepare for the following review window.
Documentation and Handover: The Tale Has To Travel
Good notes make you a much better medical professional. Poor ones wear down trust fund and connection. For PUAEME008, paperwork indicates the discomfort analysis tool utilized and ratings in time, the medications administered with dose, path, and time, the client's reaction, unfavorable impacts and activities taken, authorization discussions, and non‑pharmacological steps. It also suggests context: system of injury, position discovered, and any type of obstacles or delays.
Handover take advantage of a simple framework. I favour an adjusted IMIST‑AMBO approach for pain: Identification, Device, Injuries/illness, Indications consisting of pain ratings and vitals, Therapy given (both non‑pharm and pharmacological), and feedback. If the receiving group listens to that you titrated 20 micrograms of intranasal fentanyl to a paediatric lower arm crack, with discomfort reducing from 8 to 3, and that the kid stayed alert with secure vitals and no nausea, they promptly recognize where to choose up.
Training Pathways and That Benefits
Pain management training comes in various flavours. Brief courses hurting administration packaged around PUAEME008 generally run 1 to 2 days, with an equilibrium of concept, simulation, and functional analysis. Some companies include optional modules like laughing gas handling, or advanced splinting. A certification program hurting monitoring at this level does not provide authoritative authority by itself. It verifies capability to deliver analgesia within an organisation's scientific governance and standing orders.
For nurses who get shifts in occasion medicine or operate in country facilities, discomfort management training courses for nurses assist translate hospital‑based skills right into prehospital restrictions. Emphasis falls on limited sources, solo decision making, and documents that wrinkles smoothly right into ambulance or retrieval handover. Physio therapists working pitch‑side or in remote outreach add worth through biomechanics and gentle movement approaches. Pain management training courses for physiotherapists educate exactly how to match those toughness with safe analgesic procedures when doctors are not right away available.
Paramedic pupils usually come across PUAEME008 integrated right into their broader program. For initial -responders in the sources industry, an offer discomfort administration program might be a licensing demand before being rostered to solo protection. The pragmatic payback is clear. When I compare case reports before and after staff finish a pain administration qualification training course, I constantly see faster time to initial analgesia and fewer unintended unfavorable events. The act of exercising approval scripts, rehearsing dosing, and memorising warnings modifications behavior under stress.
Equipment and Environment: Information That Matter
You do not need a health center to supply great discomfort treatment, yet you do require dependable kit and a system that maintains it all set. Stock checklists conserve jobs. Inhalers expired last month help no one. Atomisers that do not fit your syringes hinder strategies. Include human elements. A dim stadium passage without a headlamp turns drawing up medication into a dangerous video game. A gusty roadside strips warmth from a semi‑dressed individual and presses their discomfort up while you prepare a line. Tiny touches obtain overlooked until they bite. I position a thermal blanket under and over injury individuals whenever possible, then reassess pain before I reach for drugs.

Storage and safety and security issue. Opioids require locked storage and mindful accountancy. Keep a tamper‑evident system and train every employee to use it the same way. Naloxone should sit near opioids, not buried in a different pouch. I have seen teams maintain it in an anaphylaxis package two zips far from the fentanyl. During a situation, those zips come to be canyons.
Finally, rehearse where you stand. In cramped transforming areas, make a decision ahead of time who attracts, that holds, that documents. Simulation with complete equipment deserves an hour of slides. The first time you attempt to titrate ketamine while a demonstrator's pals crowd the doorway should not be the first time you realise your screen cord is as well short for that corner.
Legal and Moral Boundaries
PUAEME008 presumes technique within an administration structure. Administrative policies and organisational methods define which representatives you can use, under what problems, and with what oversight. Discomfort administration certification does not license you to experiment. It verifies you can apply a specified method safely. Maintain copies of your extent of method, standing medicine orders, and unfavorable occasion acceleration pathway obtainable. If you function throughout organisations, anticipate variant. One employer may allow intranasal fentanyl under a scientific practice guideline. Another might limit your analgesia to oral representatives and methoxyflurane.
Ethics surface most greatly when individuals refuse treatment, when onlookers push you to rush, or when an associate urges a faster way that sneaks beyond method. Your anchor is the mix of patient autonomy, informed consent, and non‑maleficence. Decrease to carry out a medication if contraindications exist, even if the individual firmly insists. On the flip side, do not withhold analgesia as a negotiating chip for cooperation. Line up with the getting service early when you expect complicated choices. A fast phone seek advice from buys clinical and legal cover.
Building Capability: What High Quality Training Looks Like
Not all pain administration training programs cover the same ground. Try to find programs that balance pharmacology with scenario time, include devices handling drills, and call for demo of authorization conversations. A great supply pain management program includes:
- Realistic simulations that test analysis, medication preparation, surveillance, and handover with time pressure. Coverage of non‑pharmacological strategies together with pharmacology, with useful splinting drills. Clear web links to methods and range, consisting of paperwork themes and damaging occasion management. Paediatric and older grown-up considerations, with dosing variations and interaction techniques. Assessment that consists of duplicated reassessments over a situation, not simply a solitary dose and done.
As an assessor, I expect the rhythm of treatment: assess, decide, discuss, prepare, carry out, keep an eye on, reassess, paper, turn over. When students internalise that loop, their people improve care and their stress and anxiety goes down.
Common Risks and How to Prevent Them
A few patterns turn up repeatedly. The first is dealing with pain scores as design as opposed to as decision supports. If the discomfort stays high after a sensible start duration and there are no adverse indications, titrate. If the pain drops to a mild level, pivot to comfort actions and cease application. The second is equipment errors: vacant atomisers, ended vials, missing out on filters for inhalers. A pre‑shift list avoids a lot of these. The third is taking too lightly non‑drug choices. Discomfort monitoring is not a contest to see how quickly you can create fentanyl. Splint early, trainer breathing, regulate the environment, after that reach for the vial.
The most severe challenge is bad tracking. An individual who looks "comfy adequate" can still slide right into respiratory system anxiety, particularly in warm, enclosed areas or during transportation when activity lulls them. Build routines that survive distraction. Reveal your reassessment times out loud. Ask a colleague to pain management certification set a timer on the monitor or phone. Create management times on your glove if you must.
The Payoff: Faster Alleviation, Safer Treatment, Better Handover
When groups welcome the full scope of PUAEME008, scenes really feel various. Clients move from panic to participation. Extrication times shrink due to the fact that activity hurts less. Transport is calmer, handovers more clear. In audits, you will certainly see less outliers in dosing and a smoother spread of discomfort scores trending down within 10 to 15 minutes of very first contact for moderate injury. The most effective praise I have actually received after an active event change originated from a receiving nurse: "Your notes tell the story, and the person appears like the notes read."
If you are picking a pain management accreditation training course, focus on programs that rehearse the tale from very first contact to handover instead of those that just teach exactly how to press a medication. If you handle a team, embed the device into regular skills upkeep. Pain management training for nurses, physio therapists, and initial -responders is not a one‑and‑done. Protocols develop and abilities dull without use. Quarterly short drills keep the edge.
The heart of PUAEME008 is easy. Meet discomfort promptly and pleasantly, select interventions that match the person and the situation, see carefully, and tell the following medical professional precisely what happened. Do those things well and you will certainly fulfill the competency. Extra notably, you will certainly aid individuals feel secure again in mins that otherwise stretch into an eternity.